Around 2013, I was diagnosed with pre-diabetes. Doctors fear dying of the diseases they know best: gastroenterologists of colon cancer, infectious disease specialists of sepsis, you get the idea. So, for the sake of my blood sugars, after a decade-plus of abstention due to medical school, young kids, and a growing medical practice, I decided to get back into racing bicycles. I dusted off my old cyclocross bike, aired up the tires, bought some Chamois Butt’r, and congratulated myself for my reentry into competition. But note what I did not do, which is put in the miles that it takes to be a competent, competitive rider. In my first race back, a fifty-mile gravel race around Sun City, Kansas, I barely finished. If not for the help of a fellow rider who felt sorry for me, I may not even have crossed the finish line. To say the least, I had not earned my smug self-congratulatory attitude going into the race. On the drive home, the Stuart Smalley voice in my head told me I wasn’t a bad person. He told me I was human. All I had done was give myself credit for wanting to improve when I should have waited to give myself credit for actually taking the steps to improve.
I was reminded of my past foibles recently when I came across a report in the British Medical Journal pithily titled Wanting to improve is not always the same as knowing how to improve. The authors described a quality improvement project in an English hospital that aimed to reduce the length of stay of patients after knee replacement surgery. Early in the project, the investigators decided that the method of anesthesia–light sedation, heavy sedation, local anesthesia, etc.–was the primary obstacle to getting patients out of the hospital quickly. Then they went through five (five!) different anesthesia protocols over the course of seven (seven!) years. In all that time, they didn’t budge patients’ length of stay. They didn’t show an effect on any other indicator of quality, like time until the patient first walked, the patient’s reported pain, or overall pain medication use, either.
But I’m willing to bet that in that seven years, the folks involved in the study were proud of their work on improving the project, in spite of what we can see now, with the benefit of time and perspective. After all, we give ourselves credit in a number of ways that we refuse to extend to others when we have some distance from the problem, even outside of quality improvement. I may have no problem recognizing how reckless another driver is when he blasts through a fading yellow light. But when I tap the accelerator to do the same thing, since I’m generally intending to be a safe driver, it never occurs to me that my actions, too, have put other people in danger. Princeton University psychologist Emily Pronin calls this the “introspection illusion.” Our distorted self-image, blinded by the stage lights of our own personal sitcom, sees our desire to be good and ignores the fact that our objective goodness might fall short.
This intersects with the “Dunning Kruger effect,” the demonstration that the more incompetent people are, the less aware they are of their incompetence (like a slightly chubby cyclist entering his first race in years, blind to his abject lack of fitness or preparation). The more we miss the mark on a given task, the more our estimation of our success departs from reality. Physicians are especially prone to Dunning Kruger.
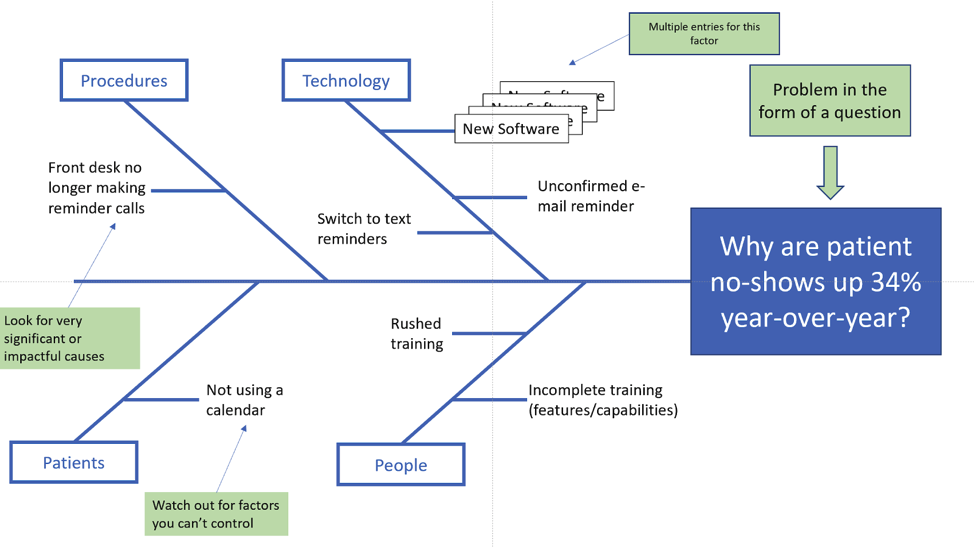
So the next time you set out to improve a process in your work, avoid the mistakes made by our English friends. First, measure the outcome you’re interested in and don’t rely on an intuitive understanding of the issue. This may require pressuring your administrative consultants to help you get meaningful data. Then put some distance between yourself and the problem through “meta-cognition.” Instead of saying, “Let’s increase the number of employees getting their diabetes screenings,” say to yourself, “Here is a company [i.e., the company you work for] in which xx% of employees received diabetes screening in the last three years.” Instead of jumping to a presumed problem to solve, think of the environment that led to the outcome you’ve measured. As Don Berwick famously said, paraphrasing others, “every outcome is the product of a system perfectly designed to achieve that outcome.” At KBGH we do this through a process called Ishikawa Analysis, first applied in post-World War II Yokohama shipyards:
https://vanguardcommunications.net/fishbone-problem-solving/
Here, the company has divided inputs into Procedures, Technology, Patients, and People. But those are relatively arbitrary. You may find you have more or fewer input classes and that they’re more process or environmentally-oriented than the example.
Next, use that loose framework to talk to employees and the health care team about what is holding them back, what we call a “stakeholder analysis.” You may have gone into the problem assuming that employees are swamping their doctors with complaints of back pain or depression, based on claims data. But you may find instead that scheduling issues aren’t allowing patients to arrive at the lab fasting before work. This process is what led the folks in the study above to a breakthrough. In talking to staff, investigators realized that, in concentrating so closely on anesthesia, they had overlooked (for seven years!) other potential contributing factors, like patient expectations, limited staff, time constraints, and cultural factors like lack of staff ‘buy in’ to the project.
Eventually, I went on to finish and do well in many, many bike races. More importantly, I lost enough weight and stayed active enough to return my blood sugars to a normal range, where they thankfully remain. And I did it not by wishing my way to better performance, but by eliminating problem foods I knew I was over-eating, increasing my fiber intake to a pre-specified goal, scheduling time to ride, working on specific skills, and measuring specific outputs. But getting modestly faster on a bicycle is trivial compared to the challenge of improving the lives of our covered employees.
As the Medical Director of the Kansas Business Group on Health, I’m sometimes asked to weigh in on hot topics that might affect employers or employees. This is a reprint of a blog post from KBGH.