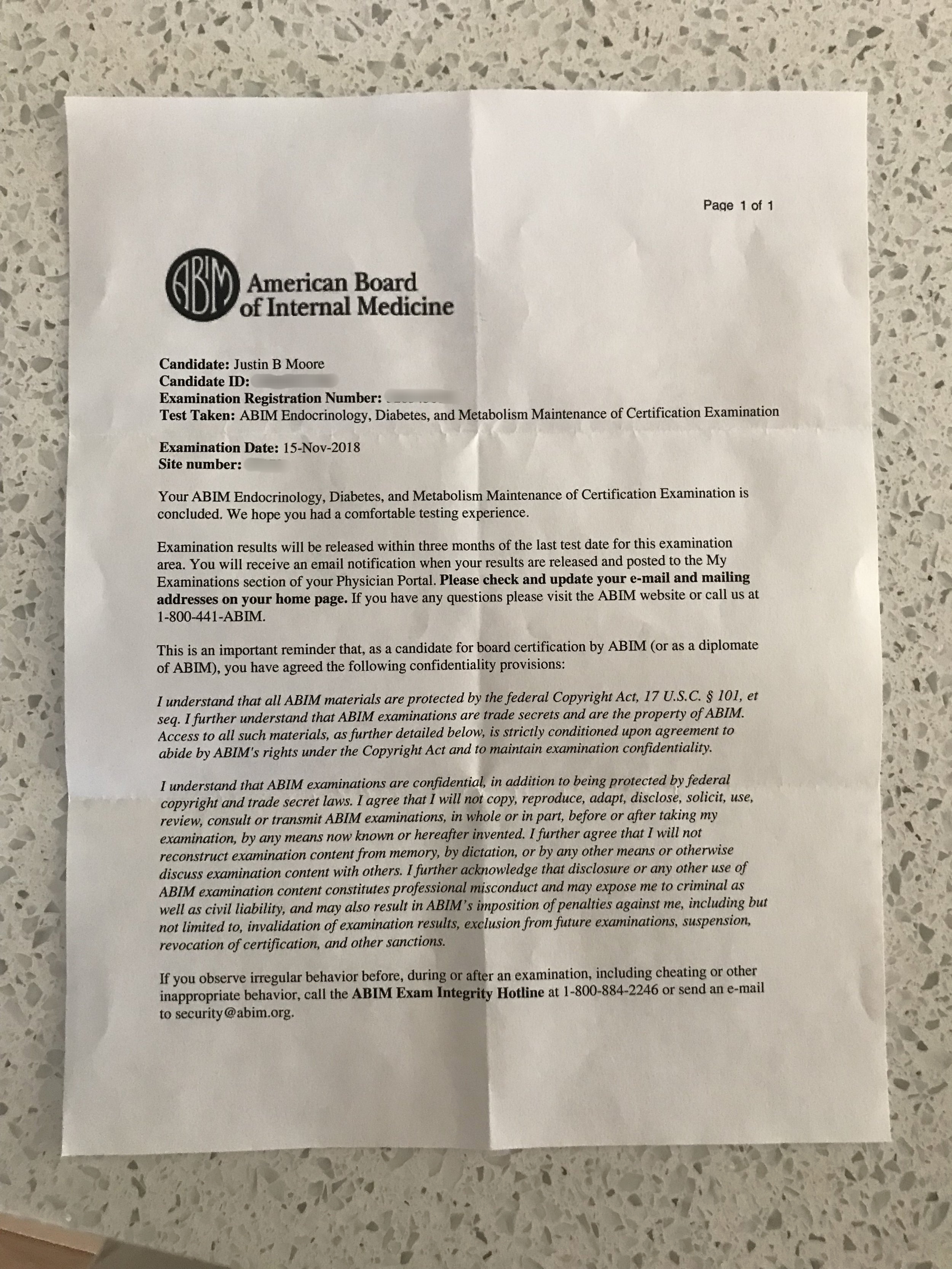
I took the ABIM endocrine maintenance exam a couple months ago.
I love the ABIM logo. It reminds me of the logo for the Southeastern Conference.
Spoiler alert: I passed. But this isn’t about my ability to pass a standardized test designed to fail only the small number of docs who can’t achieve a minimum level of competence. This post is about how good it feels to set aside the distractions of the world for a fraction of the day and really concentrate on learning something.
Ironically, the format of the exam was new. The test now includes sections in which UpToDate is available for reference. These were tricky because the availability of a reference was so seductive, much like the availability of the internet in your pocket at all times is so seductive. Lucky for me, my preparation had somewhat steeled me against this. I forced myself to use the physical version of the Endocrine Self-Assessment Program (ESAP), and I forced myself not to look up answers on the computer or my phone willy-nilly. I read through the questions, answered, read the responses, and took old-fashioned analog notes that I reviewed later. I studied around 30 minutes a day, five days/week for September and October. I kept a “30 min board review” item on my daily to-do list. I attended the Cleveland Clinic review course, which was helpful. I was amazed at the new diagnoses that have come about since I last did full-time endocrine practice. Pigmented macronodular hyperplasia? Okay then.
Analog study materials.
Ironically, I’ve somehow activated notifications on my computer so that Apple News headlines keep popping up in the corner of my screen as I’m typing this, which only serves to show how much attention residue I avoided by doing it the old-fashioned way. But even still, the first section that allowed access to UpToDate almost tripped me up. I found myself second-guessing even simple answers and clicking on the UpToDate icon to double-check myself. Even though I’m a pretty fast test-taker, and even though every UpToDate check took only a minute or so, they really added up, and I had to really hustle toward the end of that section to get done on time. For the next two sections I forced myself to finish the questions to the best of my ability and then go through any that I’d marked as potentially wrong to check them. This method left me much, much more time.
When I finished the test, mostly sure that I’d passed, I felt a sense of satisfaction that only intensified when I got my test results back. I had prepared for the test, performed well enough to pass, and legitimately increased my knowledge of endocrine diseases and their treatments. As big a pain as the board certification process is, it ultimately made me a better doctor and reinforced some of my technological minimalist views of the world.
Many of us do the same job tasks day after day. I’ve warned med students and residents about the “Groundhog Day” phenomenon. If you go into general surgery, you better like gallbladder disease, because you’re going to see it all day, every day, forever. If you become an endocrinologist you better like hyperthyroidism, because again, it’s gonna take up a lot of your day. (I would have said diabetes there, but it’s so rapidly automating that I’m not sure it will be part of the day-to-day of endocrine practice for much longer.) I’m sure the same thing is true of banking, law, manufacturing, farming, or a thousand other professions. But by going deep, you can find new sources of pleasure and satisfaction even in work that has a tendency to become rote.